Conditions I treat......... Surgery for Gait Optimisation in Cerebral Palsy
Surgery for gait optimisation in cerebral palsy is based on the premise that it is not sufficient a goal to ensure that children maintain their walking potential as they progress into adult life. Rather, the aim should be to make their walking as good as it can be by the time they are adults. Several key requirements of a satisfactory walking profile (gait profile) have been defined. I've listed these below alongside simplistic but easy to follow explanations about these terms:
- Stability in stance - the foot has to be a stable base especially during the phase of gait where we take a forward stride and there is only one foot in contact with the ground.
- Clearence in swing - the foot has to lift up as you take a forward stride and not drag against the ground.
- Adequate step length - good stride length is required for gait to purposefully get you from A to B.
- Pre-positioning foot in swing - before the advancing foot contacts the ground when taking a stride, it should be positioned to achieve stability at contact.
- Energy conservation - gait is efficient in energy terms because in essence once we get going, "controlled deceleration" of muscles regulates forward momentum rather than having to generate energy for propulsion from scratch with each step. This only works if our centre of gravity (central point in our pelvis) moves in a straight line as we walk, rather than bobbing up and down. If our joints are stiff or have reduced range of motion (like in a "pencil" man sketch), we have to "lift and drop" our centre of gravity with each step. This uses up a lot more energy leading to early fatigue and reduced walking distance. Therefore, adequate range of motion across joints and muscle balance are crucial to maintain our centre of gravity in a straight line when we are walking.
Simplistically (because this is a very complex topic), to achieve these aims we need:
- A well aligned stable foot
- No anatomical problem compromising the mechanical lever arms in our limbs -malaligned joints create "floppy" levers while bony deformity can lead to a shorter, less effective lever arm.
- Muscle balance so that our joints are supple and have adequate range of motion.
Obviously there are a lot of other important elements dictating gait. However, the two most important aspects from a functional viewpoint are muscle strength and the abillity to selectively activate muscles for a specific intended movement. Therein, lies the problem as both muscle strength and selective muscle control can not be directly improved by Orthopedic Surgery. While Orthopedic Surgery is very good at dealing with the consequences of high muscle tone - namely muscle contractures/imbalance, bony deformity and joint mal-alignment, it can't address primary muscle weakness or loss of selective control. These negative deficits (muscle weakness and loss of selective muscle control) in Cerebral palsy are often the dominant factors impairing gait rather than anatomical issues impacting on the biomechanics of gait. In cases where the negative effects of cerebral palsy are the predominant limitation, surgery for gait optimisation has to be very carefully considered. The very real concern is that the impact of surgery may make the child's gait worse (or sadly take them off their feet altogether). Multi-disciplinary assessment is crucial to make the right treatment choices that should be individually tailored for the child's functional needs.
Usually we try to reserve surgery for gait optimisation as close to skeletal maturiry as possible. The problem in cerebral palsy is that the high muscle tone is compounded by growth. Every time the child grows, the affected muscles become tighter with the risk of developing associated muscle contractures, bony deformity and joint dislocation. These effects of growth can "undo" the gains from surgery over time. By waiting for growth to be complete, we are hoping to deal with static deformities in temporal terms i.e. deformities that are unlikely to progress further in the short term. Deformity correction becomes a lot more predictable if we don't have to be worried about what changes might happen with further growth. Operating on children while growth remains carries the significant risk that with further growth, the high muscle tone will once again exert its effect and the deformity may rapidly recur. Occasionally we may have no choice but to intervene to preserve walking potential in a growing child accepting that we may need to return in the future for repeat intvention. Once again, multi-disciplinary assessment assumes vital importance in making the appropriate treatment decisions.
The multidisciplinary team
The sincere truth of good surgical outcomes in cerebral palsy is that an orthopedic surgeon can not produce these alone. (S)he, may in fact, be one of the less influential players in the team having a transient role in the overall treatment journey. Emphasis must be appropriately placed on equally (if not more) deserving members of the team:
Rehabilitation medicine - These physicians co-ordinate care of the musculoskeletal needs of patients with cerebral palsy crucially tying together all members of the care network.
Physiotherapy - Surgery can almost be viewed as an adjunctive treatment for physical therapists to achieve patient's functional goals through structured programmes following intervention.
Occupational therapy - Occupational therapists (OTs) are responsible for ensuring patient's gain maximal benefit from interaction with their physical environment whether it is home adjustments or assistive devices to help with mobility
Orthotists - A skilled orthotist works alongside the surgeon to achieve the functional objectives of surgery by delivering patient specific solutions for bracing and splintage.
Surgical techniques
Single event multi level surgery (SEMLS) hopes to achieve all the technical objectives required to optimise gait in one combined operation which may encompass operating at several different sites (levels) in both limbs. Peri-operative rehabillitation must be optimised to restore mobility and get the patient over this "single" significant surgical hit. SEMLS is preferable to several staged surgeries throughout the life of a child where each surgery will have a significant impact on the patient's mobility. Unfortunately, leaving everything to be corrected close to the end of growth is not always desirable where earlier targetted surgery may be of benefit. Ultimately, every child needs a highly individualised tailored plan of care defined by a multi-disciplinary team including Physiotherapists, Occupational therapists, Rheabilitation physicians, Orthotists and Orthopedic Surgeons.
The following list is not intended to be exhaustive as every child benefits from highly patient centred treatment taking into account their unique combination of physical examination findings, neurological deficit, general health, nutritional status, rehabilitation potential and above all personal desires and those of their care-givers. Thus there are many procedures with many variants and combinations. Nonetheless, it is useful to detail some key procedures
- Hip surgery - in walking children, hip subluxation can still be an issue and should be actively sought out. Surgery to stabilise a hip joint confers significant benefits in terms of gait efficiency and minimising the risk of progression to degenerative arthritis in the future.
- Iliopsoas lengthening - considered where there is fixed tightness across the hip. The muscle is lengthened in continuity (i.e. not divided completely) to relieve contracture but preserve strength. Usually best evaluated under anaesthetic. Often hip tightness is reactionary and will often improve when "downstream" deformities in the knee and ankle are corrected. The iliopsoas is a principle power generator in gait so best to avoid lengthening unless absolutely necessary. Therefore I try to avoid this procedure altogether.
- Femur de-rotation - Feet pointing inwards when walking does make gait inefficient and affects the lever arm of muscles around the hip. Correcting the rotational alignment of the thigh bones is best done using intramedullary devices (Rotation over a femoral nail) so that patient can return to walking as soon as comfortable.
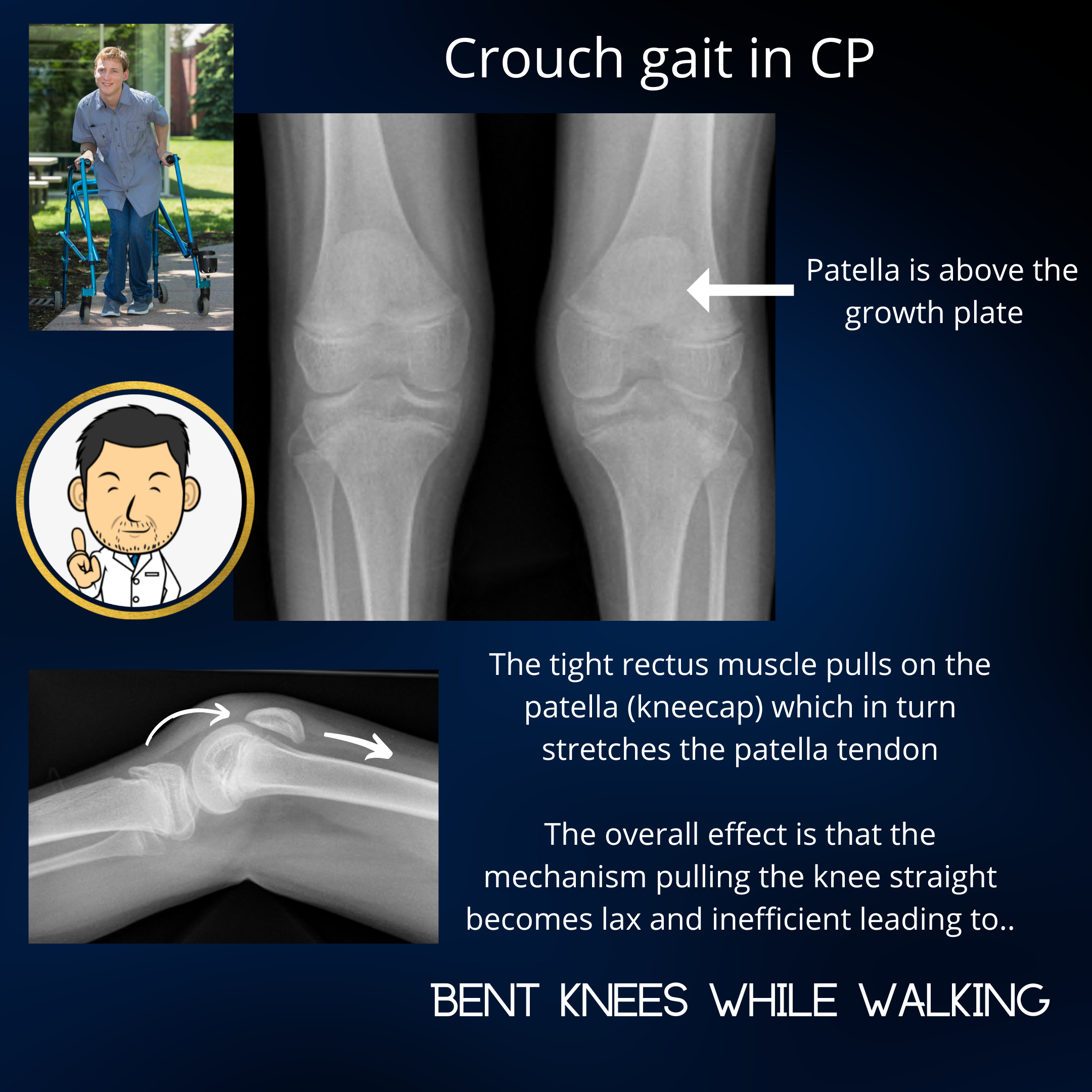
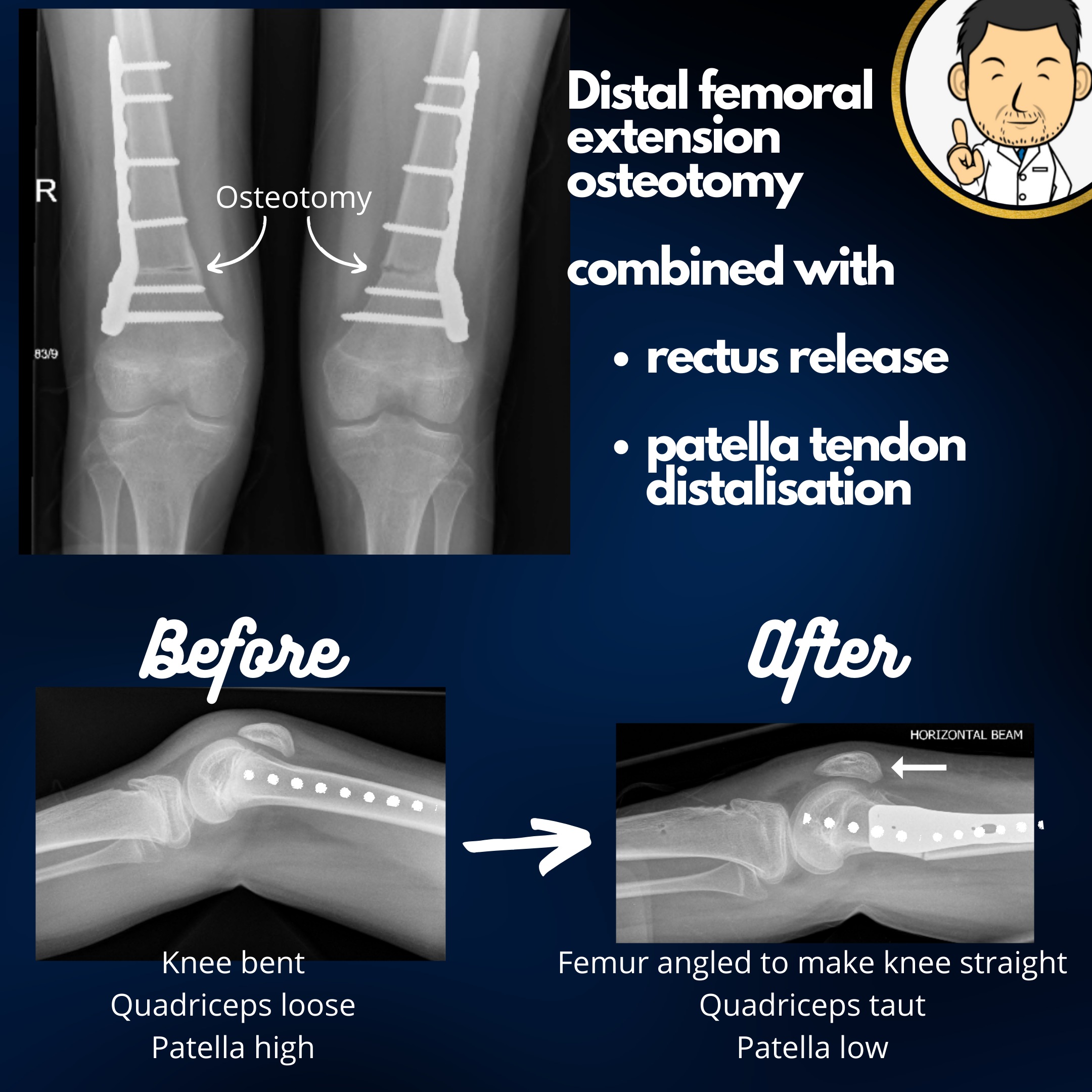
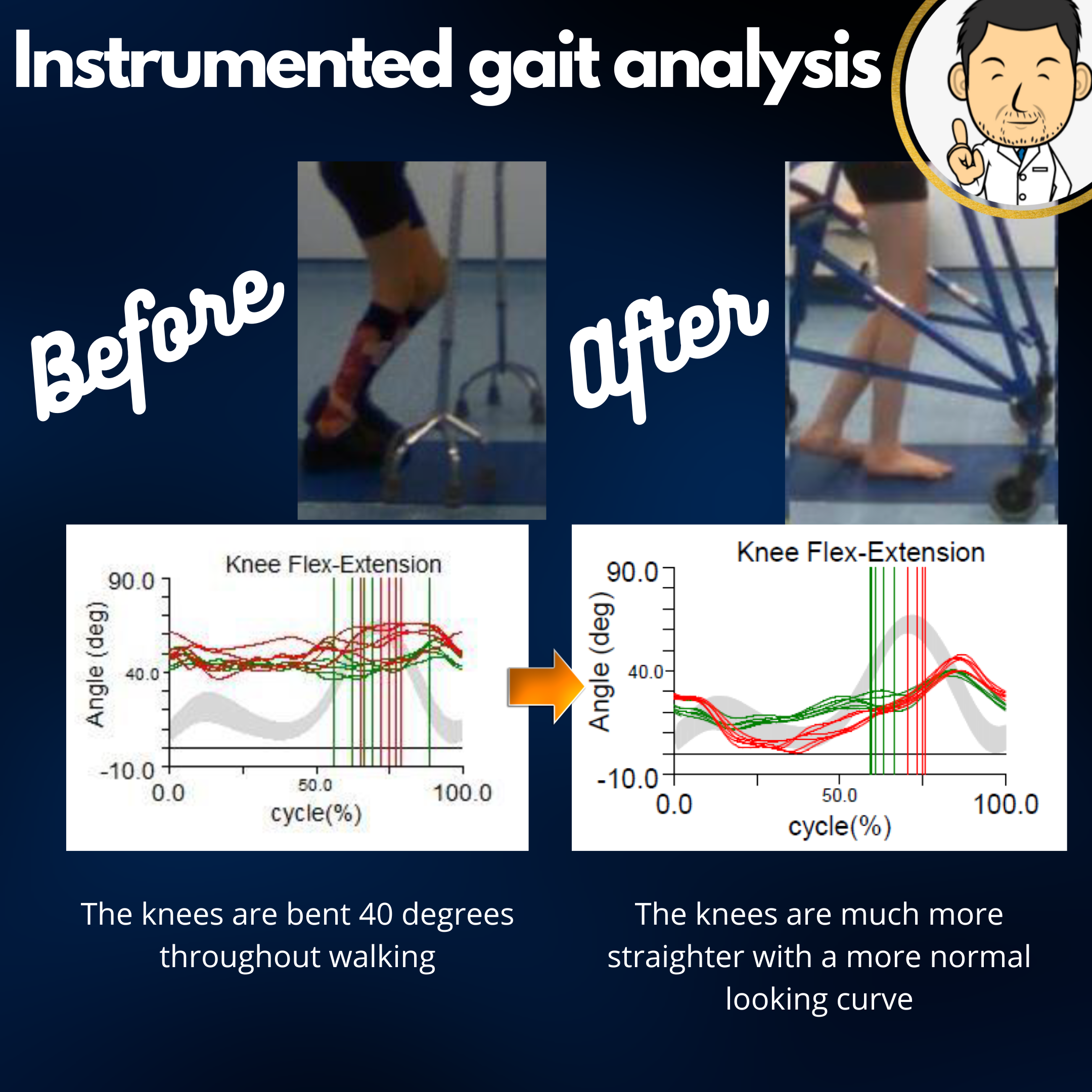
- Distal femoral extension (rotation/shortening) osteotomy (see case below) - Used to address a flexed (bent) knee gait. Rather than cutting the tendons or capsule at the back of the joint which negatively affects muscle strength, it is preferable to angulate the end of the thigh bone to make the knee come fully straight. Taking out a bit of bone when doing this angulation osteotomy is a great way of de-tensioning the tight muscles to enable the knee to come straight easily. A small amount of rotation can also be built in to correct intoeing tendency. Such bony correction is best done nearing growth completion. If significant growth remains, the bone can revert back to the original deformity quite rapidly with further growth.
- Patella tendon distalisation (see case below) - Important to be aware that the flexed knee doesn't primarily develop because the hamstring flexor muscles are too tight. Rather it is the converse situation - the quads muscles on the front have become "baggy" and redundant. Imagine a rope infront of the knee that is taut when pulling the knee straight. Now imagine what happens when you give the rope a bit of slack. Pulling on it will transfer some force to making the knee straight but likely will not produce complete knee straightening because of the redundancy. It is the same phenomenon in the flexed knee in Cerebral palsy - the quadriceps muscle on the front of the knee has become stretched out, "baggy" and redundant. Studies support the observation that restoring the normal length tension relationship of the quadriceps muscle is more important than making the knee straight. I usually undertake surgery to re-tension the quadriceps mechanism by re-attaching the tendon downstream or by transferring it's bony attachment further down the tibia.
- Rectus release/transfer - Stretching out of the quadricpes muscle is usually due to high tone in the rectus muscle - one of the four constitiuent muscles in the quadriceps (hence the name) and the only one that attaches above the hip. Selective tightness in this muscle pulls the kneecap away from the knee. This in turn stretches out the tendon connecting the kneecap to the shin bone. Taken together, the quadriceps mechanism (rectus - kneecap - tendon) over-lengthens and becomes inefficient. Releasing the rectus is an important part of treating the flexed knee and preventing it from recurring. The rectus can be transferred to other muscles after being released. However a discourse on when and why this should be done is perhaps a bit too complicated to elaborate here. The decision whether to release or transfer is best determined on a patient specific basis.
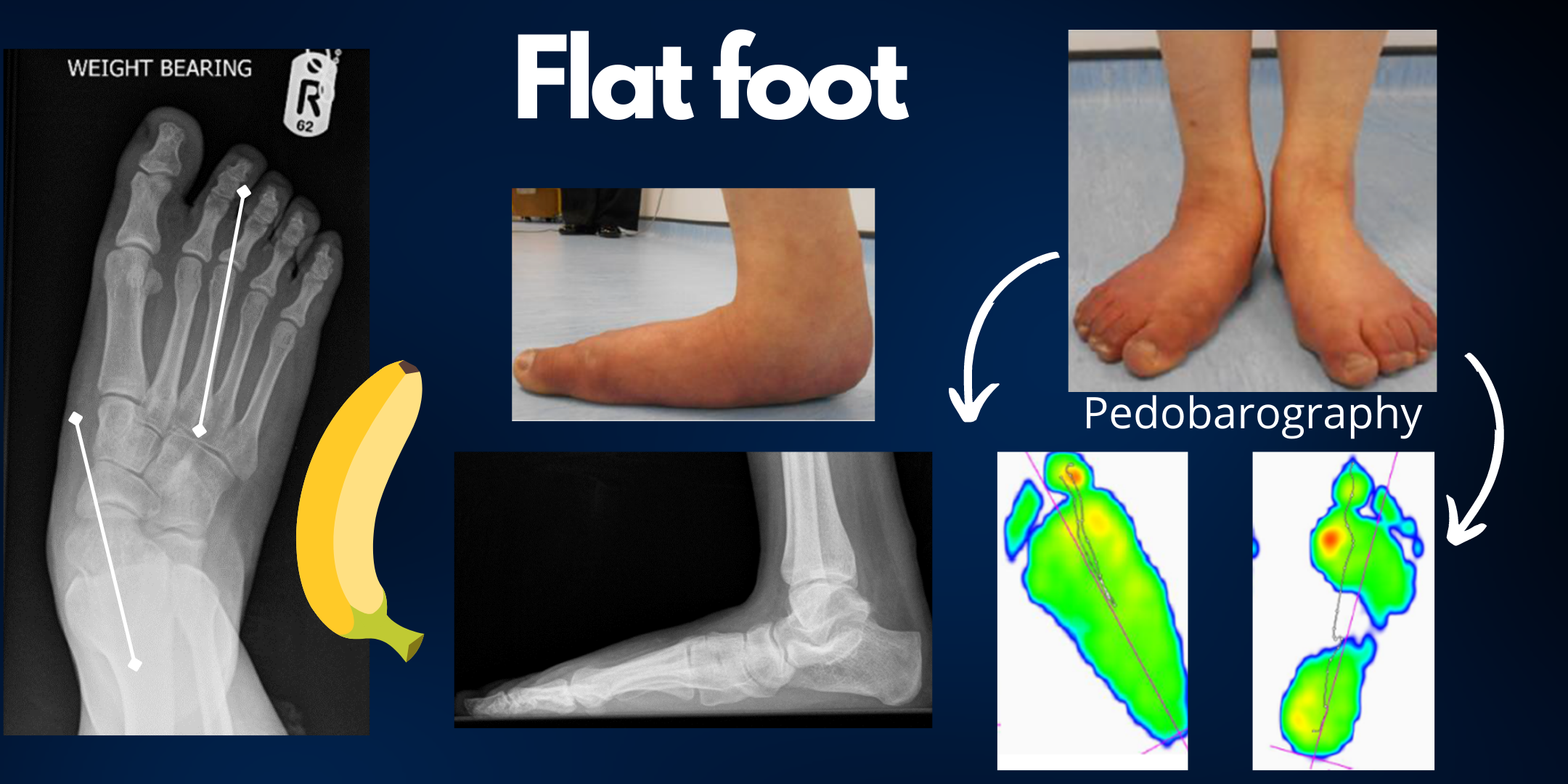
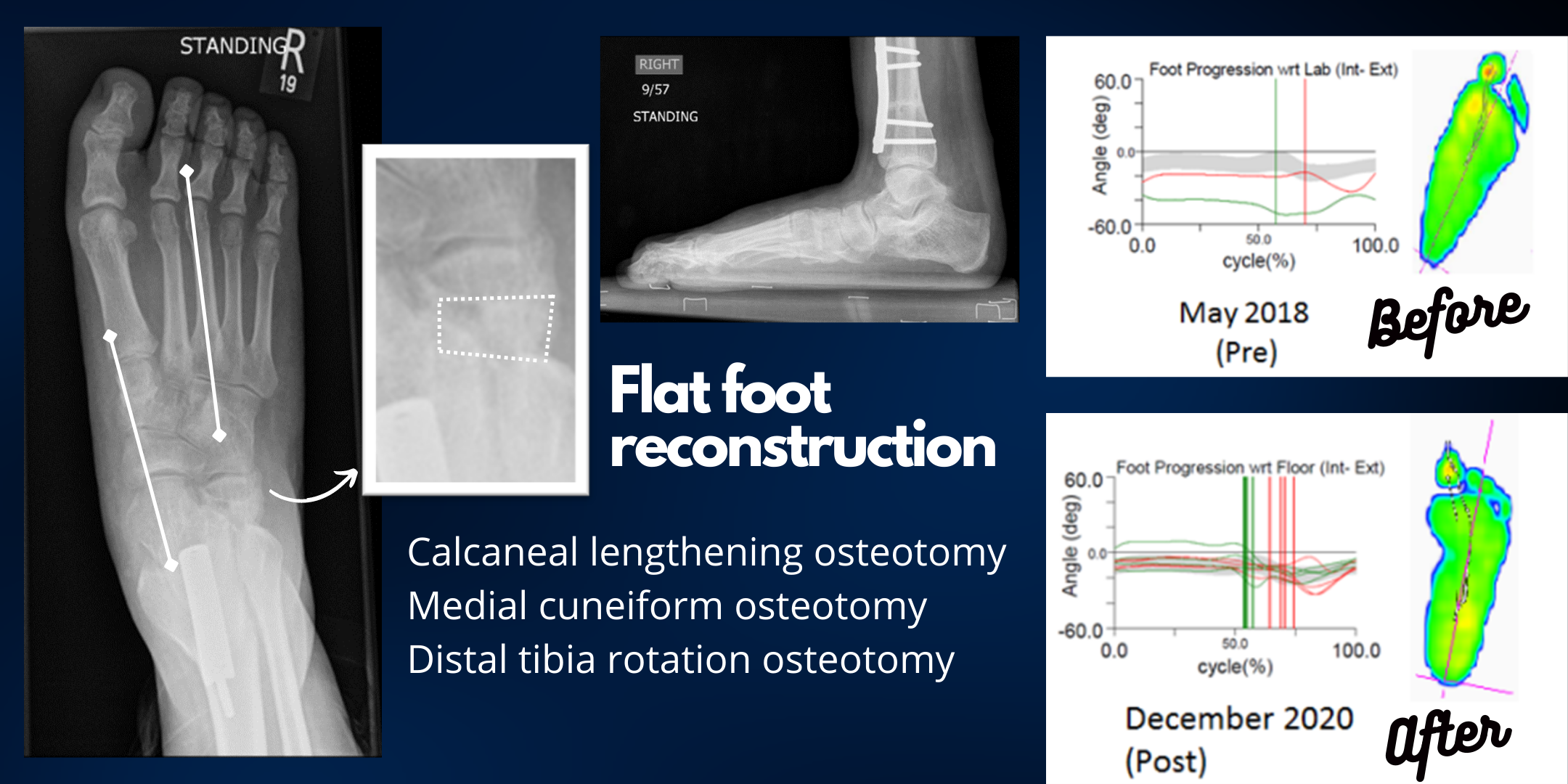
- Foot bony surgery - In young patients with excellent function, preserving the anatomy of the foot as close to normal is highly desirable. My preference for flat feet in cerebral palsy is to do a biological reconstruction with calcaneal lengthening and medial cuneiform osteotomies supplemented with tendon procedures. In patients with limited walking potential and fairly severe flatfoot deformity, a hindfoot fusion is a good option to provide a stable base for walking, especially where I feel that osteotomies would be insuffcient to correct a severe deformity.
- Calf muscle lengthening - Undertaken with considerable caution in walking children with cerebral palsy. Over-lengthening the calf muscle complex critically de-powers the ankle and pushes children who tip toe walk into a worse pattern of gait - crouch gait. "Lengthening in continuity techniques" that are calibrated to err on the side of under-correction are the preferred technique. Open surgery where the achilles tendon is completely divided before being re-attached with increased length is best avoided due to the risk of over-lengthening.
- Foot tendon procedures - These very much depend on the type of deformity and include - Tibialis anterior transfer, Tibialis Posterior recession, peroneal tendon transfer/release.